Africa has struggled to convince Western drugmakers to waive the patent rights on vaccine technology to rollout lifesaving Covid-19 jabs across the continent. Despite a range of different plans by various African countries to produce international vaccines, most of the schemes have been hit with delays relating to intellectual property rights.
Furthermore, most of the plans aspire to produce the vaccines rather than design and develop local varieties. Although the development of vaccines takes far longer than ‘fill and finish’ production, the process is important for strengthening Africa’s capacity to quickly respond to future pandemics and health concerns.
Only around 12% of Africa’s population has been fully vaccinated, putting it far behind most other regions in the world. Egypt, Ghana and Uganda are currently the only African countries to publicly state they will develop their own Covid-19 vaccines.
Egypt’s vaccine, COVI VAX, is the most advanced, having announced clinical trials in humans in November. Ghana announced in March that it would set up a vaccine research institute. Uganda has several vaccine candidates that are in the pre-clinical stages and will be tested on animals.
“We are very lucky because the government has rarely funded basic scientific research into product development,” says Sheila Balinda, a molecular virologist at the Uganda Virus Research Institute in Entebbe.
“But during Covid-19, the government decided to fund local scientists to embark on the mission of vaccine design”.
Designing a vaccine
The scientist said that her team is developing a “vector vaccine” while her colleagues are working on two other vaccine candidates: an inactivated Covid-19 vaccine and mRNA for Rift valley fever.
Vector vaccines use a modified version of a different virus known as a vector to smuggle Covid-19 spike proteins into the body which triggers an immune response, leading to the production of antibodies.
Balinda says that the vaccine candidate uses A23.1, a local strain of Covid-19 that developed in Uganda and causes mild symptoms. Her team is also developing vaccines from the more harmful Delta and Omicron strains.
“We will evaluate the performance from the individual candidates and will see which one has the best immunogenic response,” she tells African Business. “Then if any of them are not working that well we will try to make cocktails to see how the different combinations work”.
The vaccine is due to be tested in pre-clinical animal trials which will produce data to be analysed by the end of the financial year in June. The next stage is to move to clinical trials in humans.
“If our vaccine works in animal models, the next step will be getting the paperwork aligned for approvals across several local authorising bodies for clinical trials in humans,” Balinda says.
Clinical trials
The first phase of clinical trials is testing the vaccine in a sample size of around 100 people, usually healthy male volunteers. The sample size is then increased in phase two, with a longer testing period and both genders tested on to determine the doses.
Phase three is a multi-country testing period in a large sample size over 18 months. After the vaccine has been approved it will be passed to the government to begin production. The lengthy procedures mean that it will take several years before the vaccine can be manufactured at scale.
Balinda says that the lab had initially reached out to global producers with the intention of reproducing international vaccines in Uganda. In her specific case, with a vector vaccine, it would have required global drugmakers to share the exact makeup of the vaccine with Ugandan scientists.
“We wanted to get a portion of the vector from the developed world,” she says.
“We tried to contact several groups so that we could quickly come up with a local vaccine with an already generated vector. However, we could not access this outside the existing patent. This was the key motivation to develop the capacity to be able to develop this type of technology in Uganda”.
Once the vector has been developed, Balinda says that it will be patented by the government which will decide whether it can be shared freely with other African countries or not.
She adds that the difficulty in accessing vector information from western biotechnology companies was ultimately a blessing in disguise, as it encouraged Uganda to “build its capacity to ensure that we are not as vulnerable in the future”.
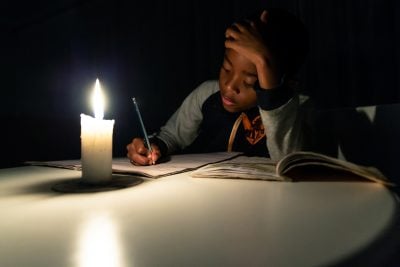
Uganda was spared the worst of the virus with only around 150,000 registered cases and less than 4,000 official deaths. The government implemented one of the world’s strictest lockdowns to protect a weak health system – with restrictions on schools, bars and nightclubs only eased in January.
Removing patents
The hesitancy of vaccine companies to share life-saving information has led to different vaccine-producing projects across Africa by different governments.
The World Health Organization (WHO) announced in February that six countries would receive training on how to produce mRNA vaccines in Africa: Egypt, Kenya, Nigeria, Senegal, South Africa and Tunisia. A global mRNA technology transfer hub was established in Cape Town last year with the aim of guiding these countries through the manufacturing process.
It was hoped that Pfizer, Moderna or BioNTech would participate in the hub but the world’s leading coronavirus manufacturers are yet to share technology – leaving the hub practically dead in the water.
Moderna has three patents against the production or sale of an mRNA vaccine in South Africa, a potential challenge for Afrigen Biologics and Vaccines, which runs the hub. The South African biotechnology firm used the publicly available sequence of Moderna’s vaccine to make its own version of the vaccine.
Other African countries have sidestepped the problem by signing deals with vaccine producers to allow them to set up local manufacturing plants, thereby removing the need for companies to share knowledge.
German biotechnology company BioNTech announced last year it would build “start-to-finish” manufacturing plants in Rwanda and Senegal to produce the mRNA Pfizer-BioNTech vaccine.
Moderna announced in March it would set up a $500m facility in Kenya to produce its vaccine. South African drug company Aspen Pharmacare signed a deal with Johnson & Johnson to manufacture its vaccine in March and distribute the one-shot jab across Africa.
Want to continue reading? Subscribe today.
You've read all your free articles for this month! Subscribe now to enjoy full access to our content.
Digital Monthly
£8.00 / month
Receive full unlimited access to our articles, opinions, podcasts and more.
Digital Yearly
£70.00 / year
Our best value offer - save £26 and gain access to all of our digital content for an entire year!
 Sign in with Google
Sign in with Google