Miners emerge from tunnels in South Africa’s North West Province each evening, faces streaked with dust and lungs heavy from the day’s toil. Before their next shift, they file into a health clinic for a quarterly lung X-ray – a ritual meant to catch tuberculosis in the early stages. Not long ago, interpreting that X-ray meant processing films and then inspecting it by eye. It took days – or even weeks – until a radiologist’s report drifted back. Now, as they button their shirts, an AI-driven triage engine has already flagged any worrisome shadows in the images.
This leap from backlog to real-time diagnosis is easing South Africa’s chronic shortage of diagnostic equipment.
The country has just five imaging units per million people, compared with an average of 18 across the 38 member countries of the Organisation for Economic Co-operation and Development (OECD), according to OECD data.
From Cape Town’s labs to Kampala’s university halls, startups and researchers are crafting algorithms that stand in for scarce specialists.
Leading this charge is Jaishree Naidoo. By early 2019 she had joined forces with strategist Terence Naidu and AI engineer Andrei Migatchev to found Envisionit Deep AI and build RADIFY, a platform that rapidly flags critical lung findings.
RADIFY reached a 700-bed Kimberley hospital within months. When Covid-19 overwhelmed the ward in mid-2020 and its sole radiologist fell ill, clinicians leaned on the software around the clock, Naidoo says.
“Seeing the tool save lives during that crisis was our real validation,” Naidoo says.
An algorithm updated weeks earlier to spot coronavirus-related pneumonia transformed a weeks-long wait into an instantaneous result.
RADIFY applies trained “convolutional neural networks” directly to digital chest X-rays, then immediately returns flagged findings, with confidence scores for these.
Safety and learning are built in from day one, says Naidoo. Whenever a human image reader challenges RADIFY’s call, the case moves into RATify, Envisionit’s monitoring platform, where radiologists review, correct and feed adjustments back into the next model update.
RATify was built to go beyond error tracking. The firm says it enables real-time validation aligned with European Union (EU) and US Food and Drug Administration (FDA) guidelines, positioning it as a regulatory assurance tool.
The technology has been designed to work on modest hospital servers. Envisionit has expanded to the UK, integrating RATify into new medical fields – proof, the company says, of global demand for African-built AI.
“Monitoring is now the big buzzword in AI,” Naidoo tells African Business, “because that’s how you ensure safety, build trust and keep your model honest.”
With $1.65m in Series A funding, Envisionit is aiming for US and EU regulatory clearance.
Challenges aplenty
Yet Naidoo’s story also lays bare the hurdles across the continent. Patchy infrastructure, unreliable power, and equipment gaps continue to slow implementation.
Kenya has one radiologist per 389,000 people; Nigeria just one per 600,000, according to a study published in the Journal of Global Health Reports. But some governments are starting to close that gap. In Rwanda, AI-powered portable X-ray machines deployed by the ministry of health are screening up to 300 people a day, including in remote areas where doctors are scarce.
These tools are helping diagnose tuberculosis early and speed up treatment, offering a glimpse of what scalable, AI-assisted care can look like.
Grand View Research estimates that South Africa’s market for AI in medical imaging will expand from $5m in 2022 to $50.1m by 2030, a 33.3% annual growth rate. Globally, the diagnostic AI market is projected to grow from just over $1.5bn in 2024 to more than $24bn by 2037, according to Research Nester.
Ayomide Owoyemi has researched in depth why so many AI-for-health pilots in Africa sputter out. Now a biomedical informatics researcher at the University of Illinois Chicago, his PhD probed the socio-technical gaps that emerge when startup ambition collides with frontline realities.
“The biggest mismatch is that people often don’t understand how things work in reality,” Owoyemi says. He points to AI chatbots built for patient engagement that ignore basic constraints – poor internet, erratic power or clinics that lack the infrastructure to keep software running.
He calls for AI tools that slip seamlessly into existing lab and billing workflows, so ministries of health or insurers will pay for them rather than leaving them to wither when funding dries up.
Yet the shortage of healthcare professionals remains stark: Africa has just 1.55 physicians, nurses, and midwives per 1,000 people – far below the World Health Organization’s recommended threshold of 4.45. In rural areas, one doctor may serve tens of thousands. These shortfalls are precisely where scalable AI tools can make the greatest impact.
While global archives such as MIMIC – a low-cost cloud-based system for medical imaging centres – provide well-curated fields of X-ray and clinical records, Owoyemi says these datasets overwhelmingly reflect white patients in North America.
Data deficit hits care
Locally-sourced, open-access data remains scarce. What does exist is often locked behind expensive licensing or housed in foreign clouds. “We need our data stored and controlled here,” Owoyemi says. “Right now, we’re relying too much on goodwill and weak privacy laws. That isn’t sustainable.”
That is exactly what Rose Nakasi is building at Makerere AI Health Lab in Kampala. Housed in the university’s College of Computing and Information Sciences, Nakasi’s lab co-designs projects with district hospitals, ethical review boards and Uganda’s ministry of health.
Interns from both computer science and public health learn to train, test and monitor models on local X-rays, feeding live data back into national surveillance networks.
“To sustain AI in healthcare, we must grow talent and oversight hand in hand,” Nakasi says. “It’s not enough to teach algorithms. We must also teach how to govern them – and where to plug them into real patient flows.” Nakasi’s lab has developed AI tools for malaria, cervical cancer, and multi-source triage and is training students to deploy them in real hospitals. But building tools is only half the challenge. To make them sustainable, they need business models that work in Africa’s fragmented, resource-stretched health systems. Naidoo knows this well. “Licensing models are easier to understand and scale,” she says. “SaaS (Software as a Service) works too. But the software must be flexible – it has to perform well on both low-bandwidth and high-bandwidth connections.”
Part of gaining trust comes from how AI is positioned – not as a replacement for overstretched doctors but as a way to help them do more with less. “That’s how the American Medical Association sees AI too: not as automation, but as augmentation,” says Owoyemi.
Investors pay attention
Across the continent, a handful of homegrown ventures are proving that AI diagnostics can thrive beyond the headline pilots.
In Nairobi, Ilara Health raised $4.2m to equip clinics with portable ultrasounds and AI-powered malaria tools, speeding up frontline treatment.
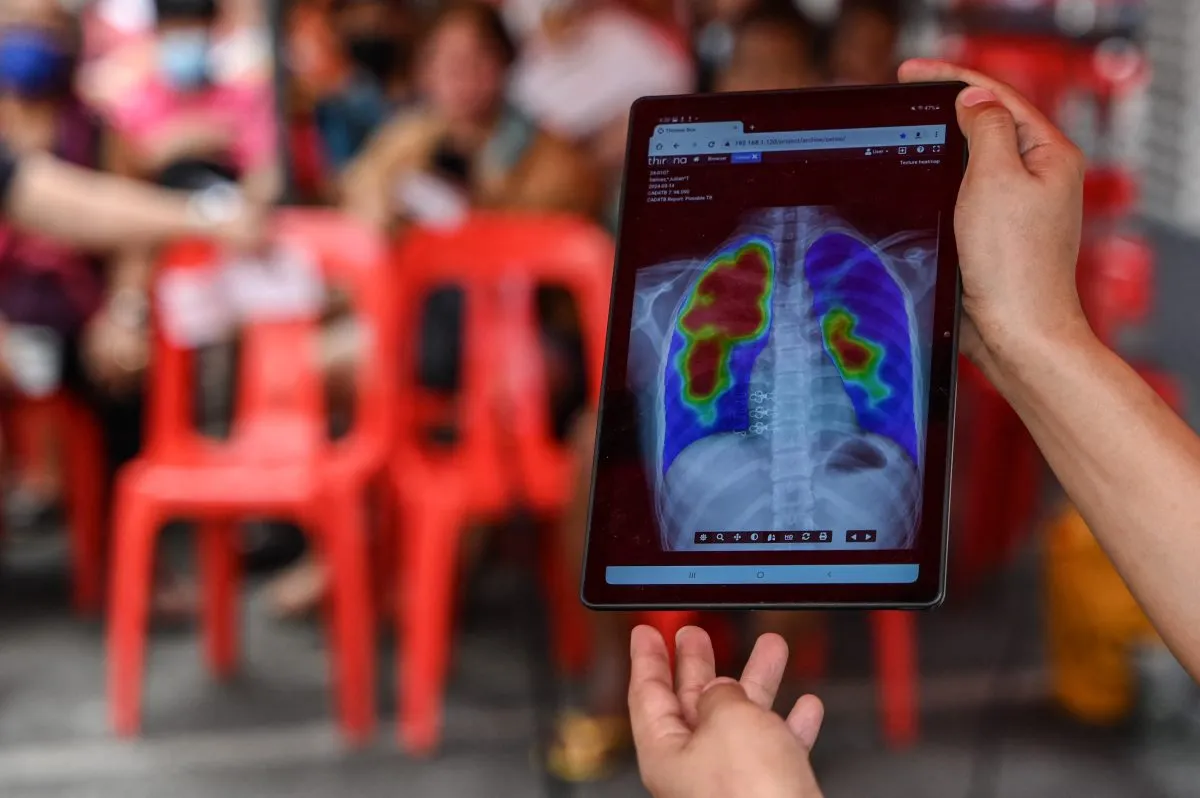
Delft Imaging’s CAD4TB platform – now integrated into national tuberculosis programmes in nine countries – secured World Bank backing.
Lagos-based Ubenwa, which built an AI model to detect birth asphyxia from newborn cries, secured $2.5m in 2022.
Such innovations show that technology must be backed by scalable business models.
Envisionit Deep AI has already partnered with mining companies to install RADIFY on site, and is in talks with private insurers to bundle AI screening into existing occupational-health packages.
For Africa’s 1.4 billion people to truly benefit from AI, these tools must be woven into systems built for the realities on the ground, not treated as plug-and-play miracles.
“You can have the smartest algorithm in the world,” Naidoo says, “but it’s worthless if the clinic loses power or the staff aren’t trained to use it.”
Want to continue reading? Subscribe today.
You've read all your free articles for this month! Subscribe now to enjoy full access to our content.
Digital Monthly
£8.00 / month
Receive full unlimited access to our articles, opinions, podcasts and more.
Digital Yearly
£70.00 / year
Our best value offer - save £26 and gain access to all of our digital content for an entire year!

 Sign in with Google
Sign in with Google