Where the vertiginous valleys of the eastern Democratic Republic of Congo (DRC) slope into Lake Kivu, a rickety barge carrying measles vaccines crosses from Goma to the city of Bukavu, where they are dispatched to a cold storage facility in the local hospital.
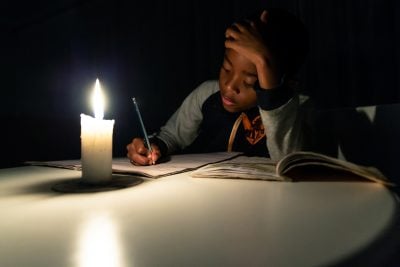
The vaccines have made their journey from India by air, but erratic electricity and stifling heat in the DRC make it hard to maintain the temperatures of 6-7C that keep the vaccines stable, says Oscar Mutama, head of vaccine distribution for South Kivu province at Médecins Sans Frontières.
“Vaccines are heat-sensitive and become less efficient if exposed to high temperatures,” he says. “In the event of a prolonged power outage, we cannot guarantee the vaccines maintain the highest quality.”
Other hospitals like Kigulube in South Kivu are in the heart of the Congolese jungle, accessible only by foot. Here hospital workers walk for hours, carrying cold boxes of vaccines to the hilltop villages of South Kivu. With most of the DRC’s major cities inaccessible by road from the capital, Kinshasa, cargo is often transported on foot or by slow-moving boats on the Congo River and its tributaries.
As Africa scrambles to access vaccines for Covid-19, a lack of cold storage and patchy infrastructure are major challenges standing in the way of distribution. Furthermore, most African countries have neither the technological capacity to manufacture a coronavirus vaccine or the money to afford them. And while rich countries battle for orders by early next year, large parts of Africa will be lucky to see the vaccine by the end of 2021, experts say.
Africa’s best bet
Two hundred and thirty-seven vaccines are currently in development around the world, according to the Milken Institute, a US think-tank. Three have released positive results in advanced trials and could be on course to receive approval soon.
The first announcement came in November through a partnership between US pharma giant Pfizer and German partner BioNtech, which jointly developed a vaccine that is 95% effective in trials. The vaccine could be out for delivery by December, the firm said, as it seeks to secure emergency US and European authorisation.
But the vaccine will provide significant logistical challenges in African countries because it requires ultra-cold storage of -70C, which is not widely available, and will spoil in five days at normal refrigeration temperatures.
The second vaccine candidate, by US biotech firm Moderna, was 94.5% effective in trials. It could be a more viable option for some African countries as it requires cooling at the more widely available temperature of -20C and will survive for up to 30 days at normal refrigeration levels.
The third – produced by AstraZeneca in partnership with Oxford University – is up to 90% effective if taken in two doses, and can be stored at standard refrigeration temperatures, although scientists say more data is needed. That could be the best option for Africa says Professor Greg Hussey, director of Vaccines for Africa, a non-profit academic unit at the University of Cape Town.
“AstraZeneca’s vaccine candidate will be more applicable than Moderna or Pfizer given the fact that we have a system in place to maintain the cold chain. We have a standard programme on immunisation, and a cold chain system in place for the living vaccines. Every country on the continent has a management system for the cold chain,” Hussey says.
Not only can AstraZeneca’s vaccine be easily transported anywhere in the world, but the British drug-maker intends to make doses available at $3-$4 each, in contrast with prices of anywhere between $10-$50 for the other two, which will make it more accessible to African nations stricken by the pandemic’s economic impact. It will be made available on a non-profit basis “in perpetuity” to low- and middle-income countries in the developing world, say the developers.
Securing the doses
AstraZeneca hopes to produce 200m doses by the end of 2020, and 700m doses by the end of the first quarter of 2021.
One of Africa’s best hopes of securing vaccines is through the Covax initiative, co-led by the World Health Organisation (WHO), the Coalition for Epidemic Preparedness Innovations (CEPI) and the GAVI Vaccine Alliance.
Since its launch in September, 180 countries have signed up to Covax, 40 of which are African low-income countries. The initiative plans to vaccinate up to 20% of the population of participating countries, with poorer countries paying only $1.60-$2 per dose. Geneva-based GAVI has secured hundreds of millions of AstraZeneca vaccines, the alliance said in a statement.
But with such high demand, Covax’s 20% goal is optimistic, and African countries might not get their populations immunised until the middle to end of 2021, Hussey says.
“Currently we know that the vaccines that are going to be produced this year and for next year will probably only be sufficient for high-income countries, because they have bought up the supply. Africa is at the tail-end of the queue. At the end of the day it’s going to be dependent on the supply-chain and manufacture of these vaccines. I would assume that by the middle-to-end of next year there may be sufficient vaccines available for many countries.”
Pfizer has engaged with governments on the continent and expressed interest in supplying Covax with doses of its vaccine that it believes could be used in the African context.
“We believe our flexible, just-in-time distribution system coupled with well-planned and organised vaccination programmes by local governments can enable reaching eligible populations across the emerging markets,” a Pfizer spokesperson told African Business.
But even if all five of the most advanced vaccine candidates gain approval, there will not be enough to protect most of the world’s population until 2022, an analysis by Oxfam recently found.
African countries must then look to their homegrown manufacturing capacity, but sophisticated biotech plants can’t be built in a day, says Hussey.
“You need a plant to make vaccines. You can’t just build a plant in a week. It could take anything up to a year or two to actually develop that capacity to make those vaccines.”
Long process
Currently South Africa and Egypt are the continent’s only contenders with the technological expertise and facilities to manufacture vaccines.
Even then, these countries would need to develop the tech-transfer processes with pharmaceutical firms to manufacture vaccines. In two related articles (see links below), we track the progress of South African firms Aspen and Biovac, which are at the forefront of the continent’s manufacturing efforts. But they may be the exceptions.
Hussey believes extending manufacturing capacity to other African countries will be a long and costly process.
“You could build a plant in the middle of Timbuktu but it requires investment by a country as well as partners of a company to build that capacity and make those vaccines and that will take a year or two.”
Want to continue reading? Subscribe today.
You've read all your free articles for this month! Subscribe now to enjoy full access to our content.
Digital Monthly
£8.00 / month
Receive full unlimited access to our articles, opinions, podcasts and more.
Digital Yearly
£70.00 / year
Our best value offer - save £26 and gain access to all of our digital content for an entire year!
 Sign in with Google
Sign in with Google